Northwell CEO: Hospital system ready for next wave
In his book Leading Through A Pandemic, Northwell Health CEO/President Michael Dowling detailed the frantic and frightening early weeks of the coronavirus pandemic. The New York City metro area was the national epicenter of the spreading virus in March and April, and he stated that his system, the largest in New York State, was the epicenter of the epicenter.
Northwell claims that it has treated more COVID-19 patients than any other medical system in the country. It has also led in vaccine distribution. On Jan. 4, Dowling stated that about 25,000 of the more than 70,000 Northwell employees had received either the Pfizer or the Moderna vaccines. He expected that number to rise quickly.
Anton Media Group interviewed Dowling in December, days before the first Northwell employee, Sandra Lindsay, RN, became the first in the nation to receive the Pfizer vaccine. She has since received her second dose and completed her vaccine regimen.
Q: What’s been the effect of the second wave on your hospital system?

A: It’s relatively modest, compared to the first wave. We have had a pretty large increase in COVID patients over the last four weeks [from 80 to 790]. We’re managing it easily. It does not put major pressure on us at all. It’s important to put that figure in context because back in April, during the height, we had 3,500 COVID patients in the hospitals. If you look at it over the last month, it’s a big increase. If you look at it compared to the first wave, it’s relatively modest.
Q: In the beginning, little was known about how to treat COVID-19. How about today?
A: We’re in much better shape than we were back in March because then we didn’t know much about the disease and the physicians and nurses were trying to figure out what it was. What parts of the body and organs it affected. What treatments might work. Over the course of the months, we’ve learned an awful lot, and today there are much better treatments. We know what to do first, we know what to do second and to do things so that patients won’t have to go into the ICU or to be intubated as much. So yes, it’s a whole different world today medically-wise than it was back in March. There are less people [percentage-wise] in ICU and being intubated, and much less mortality today than what existed prior.
Q: There was a frantic effort to get ventilators during the early stage of the first wave. Were they as big a factor as they turned out to be?
A: Not so much at Northwell. We were challenged, but we never had major difficulties back at the beginning, [compared to] other places. Today that’s not a problem, obviously. We have a stockpile of many more ventilators. We’re well equipped. And I don’t expect there to be a shortfall, irrespective of many cases we get.
Q: So the distribution warehouse you have at Bethpage is well-stocked?

A: It is completely stocked. We have adequate supplies to last a long siege there. We have plenty of masks and vents and shields. But we continue to stock it every week, because the international supply sometimes gets challenged. For example, there was problem recently in Malaysia, where some of the factories that were making gloves had to shut down for a period of time, and that constrained the shipment of gloves. So you’re always looking for different ways to get supplies. Right now we don’t expect being in any difficulty.
Q: What about your staff, is there burnout among frontline health workers?
A: The attitude is quite positive. The feedback from the workers [is that] the morale is high. There is fatigue. That’s natural. I walk around, I’m in the facilities all the time and they say to me, ‘Oh my God, I hope we won’t have to go through this again.’ But if we have to go though it again [we will]. Overall, we have a very resilient workforce. The frontline people are just terrific, the nurses and doctors and everybody, they are just wonderful. And they are ready to tackle it and beat it again. But everybody is wishing the same thing—that we wish it would be over, so that we could go back to some level of normality.
Q: What can you tell us about Northwell’s involvement with the vaccine roll out?
A: We’ve been very involved with the state Department of Health on the vaccine. We will have a major role in organizing the vaccination in this region. We are very well prepared. We have plenty of freezers to be able to keep the vaccines at the right temperatures. The freezers at Northwell have the capacity to keep 7.7 million doses and [they] are distributed across our system.
Q: As a public health official, were you surprised at how quickly vaccines were brought to market?

A: Yes, I think the speed of this process is pretty historic. But remember, a lot of the companies were working on COVID vaccines—we had MERS and SARS and H1N1, all kinds of different coronaviruses. And so there has work being done behind the scenes for a while. But yes, the speed with which they have done this and how they’ve used new technology I think is something to celebrate. And to get it approved by the FDA this quickly and they did it correctly, they did not short-circuit any of the processes—they did it the right way. So yes, that’s a very good sign.
Q: Do you see problems in dispensing the vaccine?
A: People have to remember, that to get the vaccine out to all New Yorkers, we will be vaccinating for the next six to nine months. The Pfizer vaccine is complicated to administer. It doesn’t come with pre-prepared syringes like you get with a flu shot. It comes in a compound and has to be mixed. It’s not complicated, but you have to train people how to do it. We’ve been doing that for a couple of weeks now. And the person who gets it has to stay around for about 20 minutes because there could be some side effects. Not disastrous ones, but there could be tiredness, fatigue, etcetera. So it’s not like a flu shot, when you can walk in, get the shot and get out. The reason that people don’t feel good after the vaccine is because the body is reacting to the vaccine. It’s actually a positive sign. Some people get a reaction to the flu shot. So it’s not to be unexpected. The production of the vaccine is not large enough to accommodate everybody right away. So we have to do it incrementally.
Q: There is also resistance to getting vaccinated.
A: That’s another issue. We have to do a lot of public education. A lot of people are skeptical of vaccines. They’re skeptical of this one, especially in the minority communities, who are the most vulnerable. And we just have to overcome that. And those of us in the public eye have to take the vaccine, and we talk about it and try to influence those who are skeptical that it’s the right thing to do.
Q: Governor Cuomo has been repeatedly criticized by his political opponents for being responsible for thousands of nursing home deaths in the state. Can you comment on that?

A: It’s a lot of hogwash. Did a lot of people die? Yes. It happened here. It happened in every state [and foreign countries]. They’re the most vulnerable population. Were things done here that directly caused those deaths? Absolutely not. It’s a fantastical tale that all those people died in the nursing homes because we sent them there from the hospital. That is completely false, and we’ve gone through this a thousand times. Sometimes things become so ideological, so political, that people don’t want to believe the facts. The facts are, the [virus] spread from people coming in from the community, it did not come from people put back in nursing homes from the hospitals. And the big spike in nursing homes deaths happened before there were referrals back in nursing homes. It’s unfortunate that a lot of elderly people died and the governor has indicated that he’s very unhappy about that as well, and everybody should be, irrespective of your politics. But if you look at other states, they’ve all had dramatic deaths in nursing homes. They’re the most vulnerable people. And some nursing homes did not prepare as properly as they should have. Those kinds of criticisms are going to fly—I don’t get overly bothered by them.
Q: Do you think your book can become a template for other systems and even single hospitals on how to fight future pandemics?

A: At Northwell, we were prepared better than most. But the big challenge for every hospital right now and for every government at all levels is to not forget that when this is over, to start preparing for the potential of another one. Memories are short. So when the crisis is over, people might relax and go back to the old ways—you can’t go back. So we have to do a lot of different things going forward. We have to put more emphasis on science and invest in science and more research. We have to develop more domestic manufacturing of PPEs—we can’t be partially reliant on overseas. We have to put infrastructure in our facilities so that we ware better prepared the next time there is a crisis. So, these are the kind of things that have to be dealt with going forward, once we get out of this. Because we will have another pandemic. Populations are expanding into non-habitated areas and you’re going come into contact with animals and other sources of potential disease. We’ll have more. They may not be as bad as this one—they won’t last this long. If you go back over [the past decade] you had SARS, you had MERS. Everybody’s been predicting that we would get what we got. There was no one completely prepared for this. But we’d better be prepared in the future.
Q: The medical regulatory reforms the governor introduced during the emergency, will they get put into practice when things go back to normal?
A: Many of the reforms I’ve been pushing should continue. I would hope that we don’t go back and put into place regulations that we should have never have had to begin with. The state and federal governments have to be careful not to overly micromanage. That is a recipe for disaster. And the state has indicated that they want to dispense with some of the regulations forever, of the things that don’t make any sense. I would hope that would happened, but you know bureaucracies are bureaucracies. They could go back to the way they were.
Q: The new nurses and physician assistant that were rushed into service at the start of the crisis—did you feel that they performed up to par? Was it encouraging?
A: It’s very encouraging. Everybody that we put into service, including regular physicians and nurses that don’t work in the ICU, and the medical students and nursing students that we wound up putting in the ICU, everybody performed view wonderfully in my view. Without them we would have been in difficulty. And the pandemic forced different medical disciplines to work more closely, and hopefully, we’ll be able to continue that trend post-COVID. I can’t say enough about the people on the front lines here.
Q: Do you think there will be changes in medical education to enable future health care workers and physicians to be able to face these type of situations?
A: Yes, I think the educational programs and medical schools are all adapting now to what’s needed in these situations. And we’ll always be looking right now at staff to prepare them in the future if this gets bad over the holiday season. But we may need to deploy them back to the work that they did before. It’s been an education for everybody. They’ve enhanced their capabilities as a result. When you’re put into a new situation, you learn very quickly. COVID is going to change everything. You have to be different going forward. And I think quite frankly we’re going to be in many ways better off because of COVID in some aspects. Obviously, it’s had a major economic toll. But I do think it’s going to force us to reimagine our organizations differently going forward.
Q: COVID took a toll on your system’s finances. Are you looking for some kind of federal help down the road?
 A: We took a major hit financially in terms of overall revenue for the last four or five months. We did get some federal help, but it did not close the hole, however. We are expecting and we’re optimistic about the potential for some other federal help. But we’re moving forward. We’ve completed our budget for 2021 and we’ll come back strong. And we’ll welcome all new help that we can get. But if doesn’t come through we have to manage to the best of our ability and get us back in a sure footing. We’re a strong organization. We will be strong as a result of this—I’m not worried about that at all right now.
A: We took a major hit financially in terms of overall revenue for the last four or five months. We did get some federal help, but it did not close the hole, however. We are expecting and we’re optimistic about the potential for some other federal help. But we’re moving forward. We’ve completed our budget for 2021 and we’ll come back strong. And we’ll welcome all new help that we can get. But if doesn’t come through we have to manage to the best of our ability and get us back in a sure footing. We’re a strong organization. We will be strong as a result of this—I’m not worried about that at all right now.
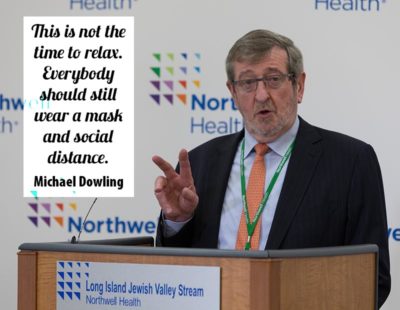
Q: Any final thoughts?
Q: The fact that we have a vaccine is great news [but] it’s going to take a long time for the roll out. And if you gave someone a shot today, they’ll have to take a second one three weeks from now. It doesn’t begin to take effect for up to six weeks. My point is this is not the time to relax. Everybody should still wear a mask and social distance. Should still wash their hands. If people relax on that because the vaccine is here, that will only prolong the COVID crisis. The crisis will last as long as the public decides not to comply. If the public complies, we will get this crisis over very quickly. Back in March or April, if the federal government had emphasized mask wearing for everybody, and use the White House as a bully pulpit to [spread the message], we would be in a better position today.